Chronic pain affects millions globally, persisting beyond normal healing timeframes and often without clear physical cause, significantly impacting quality of life. Unlike acute pain serving protective functions by signaling injury, chronic pain becomes a disease itself with complex neurological, psychological, and social dimensions. Traditional medical approaches focusing solely on symptom suppression through medication often prove inadequate or create dependency problems. Comprehensive pain management integrates multiple modalities addressing biological, psychological, and lifestyle factors, empowering patients as active participants rather than passive recipients of treatment. Understanding pain mechanisms and evidence-based interventions enables more effective management even when complete elimination remains impossible.
Medical Interventions and Medication Strategies
Non-opioid medications including acetaminophen and NSAIDs provide first-line treatment for many pain conditions with lower addiction risk than opioids, though long-term use requires monitoring for liver or kidney effects. Topical analgesics deliver medication directly to painful areas, reducing systemic exposure and side effects. Antidepressants and anticonvulsants, originally developed for other conditions, effectively treat certain chronic pain types by modulating neurotransmitters involved in pain processing. Opioid medications remain appropriate for severe pain unresponsive to other treatments, though require careful management balancing pain relief against addiction, tolerance, and side effect risks. Interventional procedures from nerve blocks to spinal cord stimulation interrupt pain signals when conservative treatments fail, offering alternatives to surgery or long-term medication. Physical therapy strengthens supporting muscles, improves flexibility, and teaches body mechanics reducing strain on affected areas. Occupational therapy adapts daily activities and environments minimizing pain triggers while maintaining function and independence. However, medication alone rarely provides complete chronic pain relief, making multimodal approaches essential for optimal outcomes.
Psychological and Behavioral Approaches
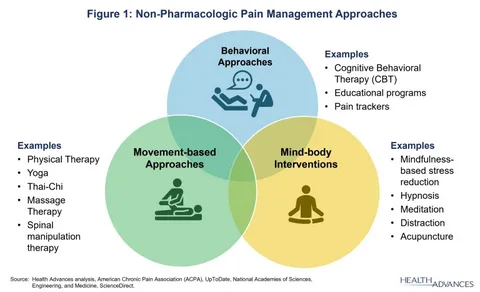
Cognitive behavioral therapy helps patients identify and modify thought patterns and behaviors that amplify pain perception and disability, improving coping regardless of pain intensity. Mindfulness meditation trains attention on present-moment experience without judgment, reducing suffering associated with pain even when sensation intensity remains unchanged. Acceptance and commitment therapy focuses on valued activities despite pain rather than eliminating discomfort, shifting goals from cure to meaningful living. Biofeedback teaches conscious control over physiological processes like muscle tension and stress responses that exacerbate pain. Relaxation techniques including progressive muscle relaxation and guided imagery reduce physical tension and anxiety often accompanying chronic pain. Sleep hygiene improvements address the bidirectional relationship between pain and poor sleep, as better rest reduces pain while pain disruption prevents restorative sleep. Pacing strategies balance activity and rest preventing boom-bust cycles where overexertion during good days triggers flares requiring extended recovery. Social support from family, friends, or support groups combats isolation and provides practical assistance and emotional validation. Depression and anxiety commonly accompany chronic pain, requiring treatment addressing mental health alongside physical symptoms for comprehensive care.
Lifestyle Modifications and Alternative Therapies
Regular exercise paradoxically reduces many chronic pain conditions despite initial discomfort, with low-impact activities like swimming, walking, or cycling improving fitness without excessive joint stress. Weight management reduces mechanical strain on weight-bearing joints while decreasing inflammatory processes contributing to pain. Anti-inflammatory diets emphasizing whole foods, omega-3 fatty acids, and antioxidants may reduce systemic inflammation though evidence remains mixed for specific conditions. Ergonomic workplace adjustments prevent repetitive strain and postural stress that aggravate pain conditions. Heat therapy relaxes muscles and increases blood flow while cold therapy reduces inflammation and numbs acute pain, with optimal choice depending on condition type. Massage therapy provides temporary relief and relaxation though benefits typically don’t persist long-term without ongoing treatment. Acupuncture demonstrates effectiveness for certain pain types in quality research, though mechanisms remain debated and individual responses vary considerably. Yoga and tai chi combine gentle movement, strength building, flexibility, and mindfulness with evidence supporting benefits for various chronic pain conditions. Ultimately, effective chronic pain management recognizes that complete cure may not be possible, instead focusing on maximizing function, minimizing suffering, and maintaining quality of life through personalized combinations of medical, psychological, and lifestyle interventions adjusted over time as needs and responses evolve.